<h2>Medicare Advantage Organization And Former Chief Operating Officer To Pay $32.5 Million To Settle False Claims Act Allegations</h2>
<p>Tampa, FL – Freedom Health Inc., a Tampa-based provider of managed care services, and its related corporate entities (collectively “Freedom Health”), agreed to pay $31,695,593 to resolve allegations that they violated the False Claims Act by engaging in illegal schemes to maximize their payment from the government in connection with their Medicare Advantage plans, the Justice Department announced today. In addition, the former Chief Operating Officer (COO) of Freedom Health Siddhartha Pagidipati, has agreed to pay $750,000 to resolve his alleged role in one of these schemes.</p>
<p>“Medicare Advantage plans play an increasingly important role in our nation’s health care market,” said Acting U.S. Attorney Stephen Muldrow. “This settlement underscores our Office’s commitment to civil health care fraud enforcement.”</p>
<p>“When entering into agreements with managed care providers, the government requests information from those providers to ensure that patients are afforded the appropriate level of care,” said Acting Assistant Attorney General Chad A. Readler of the Justice Department’s Civil Division. “Today’s result sends a clear message to the managed care industry that the United States will hold managed care plan providers responsible when they fail to provide truthful information.”</p>
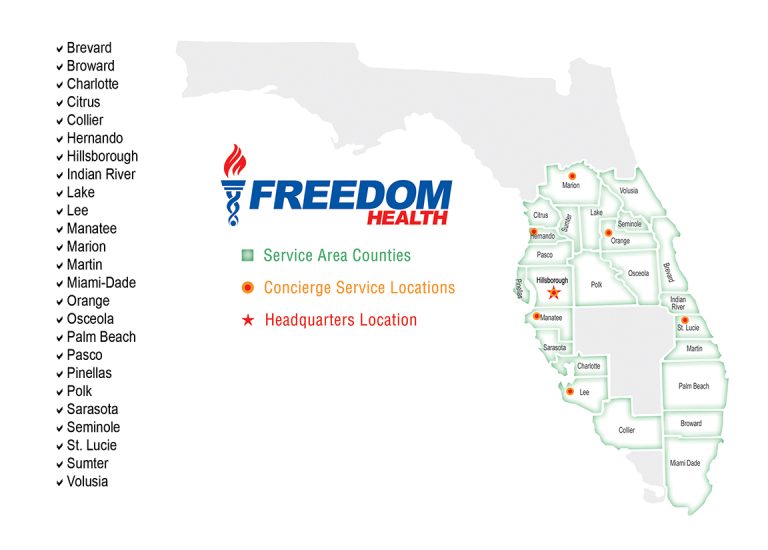
<p>The government alleged that Freedom Health submitted or caused others to submit unsupported diagnosis codes to the Centers for Medicare &; Medicaid Services (CMS), which resulted in inflated reimbursements from 2008 to 2013 in connection with two of their Medicare Advantage plans operating in Florida. It also alleged that Freedom Health made material misrepresentations to CMS regarding the scope and content of its network of providers (physicians, specialists and hospitals) in its application to CMS in 2008 to expand in 2009 into new counties in Florida and in other states. The government’s settlement with Mr. Pagidipati resolves his alleged role in this latter scheme.</p>
<p>“Medicare Advantage insurers must play by the rules and provide Medicare with accurate information about their provider networks and their patients’ health,” said Chief Counsel to the Inspector General Gregory Demske of the Department of Health and Human Services Office of Inspector General (HHS-OIG). “OIG will investigate and hold managed care organizations accountable for fraud. Moving forward, the innovative CIA reduces the risks to patients and taxpayers by focusing on compliance issues unique to Medicare Advantage plans.”</p>
<p>The allegations resolved by these settlements were brought in a lawsuit under the qui tam, or whistleblower, provisions of the Federal False Claims Act and the Florida False Claims Act. These statutes permit private parties to sue on behalf of the government for false claims and to receive a share of any recovery. The whistleblower in this action is Darren D. Sewell, who was a former employee of Freedom Health. The whistleblower’s share in this case has not yet been determined.</p>
<p>The corporate entities related to Freedom and which were part of today’s settlements are: Optimum HealthCare Inc., America’s 1st Choice Holdings of Florida LLC, Liberty Acquisition Group LLC, Health Management Services of USA LLC, Global TPA LLC, America’s 1st Choice Holdings of North Carolina LLC, America’s 1st Choice Holdings of South Carolina LLC, America’s 1st Choice Insurance Company of North Carolina Inc. and America’s 1st Choice Health Plans Inc.</p>
<p>Today’s settlements were the result of a coordinated effort by Assistant U.S. Attorneys Katherine Ho and Randy Harwell of the Middle District of Florida, Trial Attorney Jennifer Koh of the Department of Justice’s Civil Division’s Commercial Litigation Branch, HHS-OIG and Assistant Attorney General Ian Garland of the Florida Office of the Attorney General.</p>
<p>The claims resolved by the settlements are allegations only, and there has been no determination of liability. The case is captioned <u>United States ex rel. Sewell v. Freedom Health, Inc., et al.</u>, Case No. 8:09-cv-1625 (M.D. Fla.).</p>
<p><a href="https://www.justice.gov/usao-mdfl/pr/medicare-advantage-organization-and-former-chief-operating-officer-pay-325-million">Original PressReleases&#8230;</a></p>

Healthcare Fraud: Freedom Health Inc., Agreed to Pay Engaging in Illegal Schemes to Maximize Their Payment From The Government in Connection With Their Medicare Advantage Plans
Medicare Advantage Organization And Former Chief Operating Officer To Pay $32.5 Million To Settle False Claims Act Allegations
FraudsWatch is а site reporting on fraud and scammers on internet, in financial services and personal. Providing a daily news service publishes articles contributed by experts; is widely reported in thе latest compliance requirements, and offers very broad coverage of thе latest online theft cases, pending investigations and threats of fraud.
Leave a Comment


The Ultimate Guide to Avoiding Online Scams
Stay safe online! Our comprehensive 2025 guide covers phishing, AI scams, investment fraud & more. Learn red flags, prevention steps & how to report scams. Protect yourself now via Fraudswatch.com.
Read More
Categories
- AOL Aim Live ATT
- Celebrities Scammed
- Credit Card
- Credit Scam
- Email Man-Male Scammers
- Email Scam List
- Email Scams Examples
- Fraud
- Fraud News From World
- Fraud Prevention
- Gmail.com
- Hotmail.com
- Insurance
- Jobsearch Scams
- Loans
- Military Scammer
- Mortgage
- Nigerian 419
- Report Fraud
- Romance Scammer
- Russian Email Scam
- Scammer
- Scams Ways
- Shopping & Saving Money
- Spam
- White-Collar Crime
- Yahoo.com
Recent Posts
- Bulletproof Betrayal: Inside the $5.2 Million ShotStop Fraud That Sold Counterfeit Body Armor to America’s Law Enforcement July 8, 2025
- The Weapon of Experience: Inside the $28M Memphis Pharmacy Fraud and a Prior Conviction at the Heart of a Record-Breaking National Takedown July 2, 2025
- Chicago Businessman Convicted in $55 Million Fraud Scheme Targeting COVID-19 Relief Funds and Financial Institutions July 2, 2025
- Betrayal in the Classroom: An In-Depth Analysis of the Unprecedented Criminal Charges Against the School District of Philadelphia for Asbestos Failures June 28, 2025
- Anatomy of a Scandal: How a NY Governor’s Aide Allegedly Masterminded an $8M COVID PPE Fraud and Kickback Scheme June 28, 2025
Tags
Bank Fraud
Banking Fraud
Bankruptcy Fraud
Bribery Scheme
Business Fraud
Celebrities Scammed
Charity Fraud
Commodities Fraud
Consumer Fraud
Consumer Protection
COVID-19 relief fraud
Credit
Credit card
Credit Card Fraud
Credit Repair
Credit Repair Scams
Crime
Cyber Crime
Cybercrime
Cyber Criminals
Cybersecurity
data breach
Dating Scammer
Elder Fraud
Elder Justice
Email
Email Letter
Email Scam
Email Scam Examamples
Email Scam Example
Email Scam Examples
Email Scams
Email Scams Examples
False Claims Act
FBI
Fedex
Financial Crime
Financial Fraud
Fraud
fraud prevention
Fraud Scheme
Health
Health and Wellness Scams
Health Care Fraud
Healthcare Fraud
Identity Theft
Immigration Fraud
Insurance
Insurance Fraud
Internet Fraud
Investment Fraud
job
Job Scam
job scams
Loan
Loan Fraud
Loan Scam
Loans Fraud
Lottery Scam
Mail Fraud
Medicare Fraud
Microsoft
Military Scammer
Military Scammer LT. JEFFREY MILLER
Military Scammers
Money Laundering
Money Laundering Scheme
Mortgage
Mortgage Fraud
Mortgage Scam
Mortgage Scams
National Security
Nigerian
Nigerian 419
Nigerian Scam
online fraud
Online Scams
PayPal
personal information
Phishing
Phishing Scams
Ponzi Scheme
Public Corruption
Ransomware
Report Fraud
Romance Scam
Romance Scammer
Romance Scammers
Romance Scams
Scam
Scammer
Scammers
scams
Securities Fraud
spam
Tax Evasion
Tax Fraud
Travel Scams
White Collar Crimes
wire fraud